Since April 2023, the Department of Public Health and Human Services (DPHHS) has been determining eligibility for Medicaid recipients. During the pandemic, the federal government paused the requirement that states periodically recertify Medicaid eligibility, and recipients were allowed to receive continuous coverage from 2020 to the spring of 2023.
This process, known as the “unwinding” has resulted in 120,707 Montanans, including 12,857 American Indians, losing health insurance thus far. The vast majority – 64 percent - have had their coverage terminated due to procedural reasons, like returning incomplete paperwork, and not because they were ineligible.
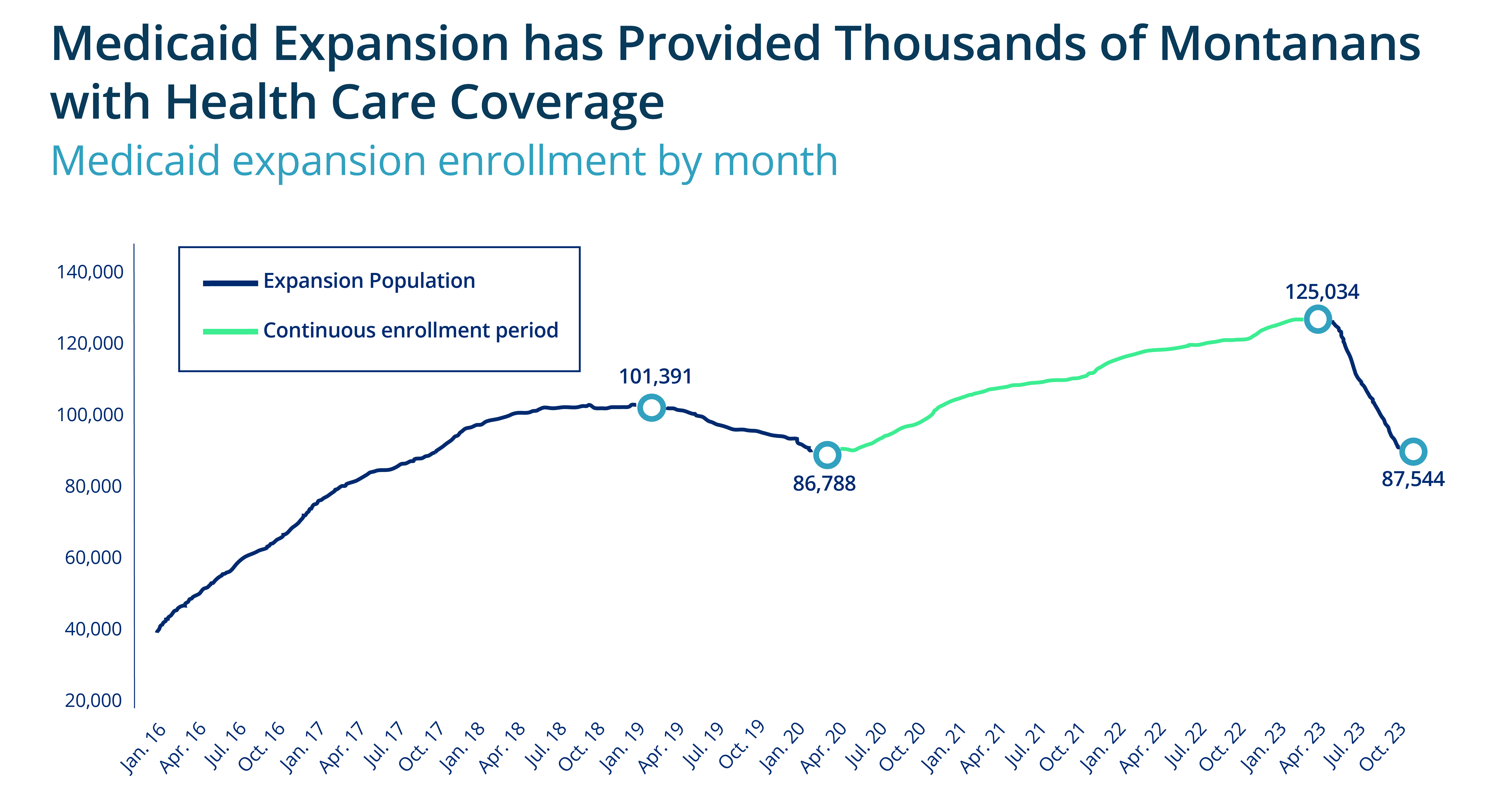
In 2025, Montana legislators will need to vote to renew Medicaid expansion. The administrative chaos of unwinding gives us a small preview of the hardships that ending expansion could create. Montana should use this opportunity to renew Medicaid expansion, and strengthen the program for long-term success.
Communication
With nearly two-thirds of recipients unable to renew their Medicaid due to procedural problems, the need for DPHHS to improve communication with recipients should be one of the top lessons learned from the unwinding. Legal notices from state agencies can be difficult for users to understand, and DPHHS should ensure all communications are accessible.
Improving communications could include
• Consulting with advocates on the readability of notices;
• Ensuring language accessibility;
• Gathering recipient feed back through surveys, focus groups, and evaluations;
• Performing multiple follow-up opportunities via e-mail, text, or phone calls.
When it became clear a high number of individuals were failing to return their Medicaid redetermination packets, DPHHS should have paused the unwinding and addressed the underlying communication barriers. Moving forward, the state should use this opportunity to improve communications with benefit recipients.
Access
A significant lack of access to information and assistance from DPHHS contributed to individuals being unable to renew their Medicaid coverage. Due to budget cuts enacted in 2017, Montana closed 19 Offices of Public Assistance, limiting the number of places Montanans could receive in-person assistance.
During the unwinding process, Montanans also encountered significant difficulties calling the Public Assistance Help Line, with many reporting hours-long wait times. Likewise, recipients reported trouble navigating the www.apply.mt.gov website and encountering frequent glitches.
To improve Montanans’ ability to access enrollment assistance, DPHHS should:
• Consider reopening Offices of Public Assistance;
• Improve staffing for the Public Assistance Help Line; and
• Ensure www.apply.mt.gov is functional and accessible for users.
Administrative Process
Montana’s unwinding has highlighted areas where the state’s administrative process falls behind the rest of the nation. For example, in October of 2023, Montana renewed only 19 percent of redeterminations on an ex parte basis (that is, using available data rather than relying on individuals to self-report), less than half the rate of the national average. Furthermore, Montana’s Medicaid application processing time far exceeds federal regulations, with 31 percent taking longer than 45 days to process. Montana is also seeing a record number of Medicaid applications, suggesting many of those who lost coverage were, in fact, still eligible and needed to reapply.
Improving DPHHS administrative efficiency could look like
• Renewing continuous eligibility to reduce the number of Medicaid redeterminations to process;
• Improving the use of available data to renew (ex parte); and
• Sufficiently educating and staffing eligibility positions.
Looking Forward
The unwinding has highlighted the importance of Medicaid to individuals, providers, and our broader health care community. Moving forward, DPHHS should use the lessons learned from the unwinding as an opportunity to strengthen our Medicaid program to make it more efficient and accessible for participants. To read more about Medicaid expansion, read our newest report: Medicaid Expansion in Montana.

MBPC is a nonprofit organization focused on providing credible and timely research and analysis on budget, tax, and economic issues that impact low- and moderate-income Montana families.